Bulk Bill Claims (Online Claiming)
Use the tab to manage claims bulk billed to Medicare using Medicare Australia's online claiming, where the cost of the encounter is covered by Medicare.
Encounters list
- Have a provider with a valid provider number or have a claim item set
- Are not marked as Not claimable (see Service Record for details)
- The patient is not fictitious
- The encounter status is waiting, started, paused or finished (but not withdrawn)
- Have not been paid
- Are within the legal time limit for electronically claimable services imposed by Medicare Australia
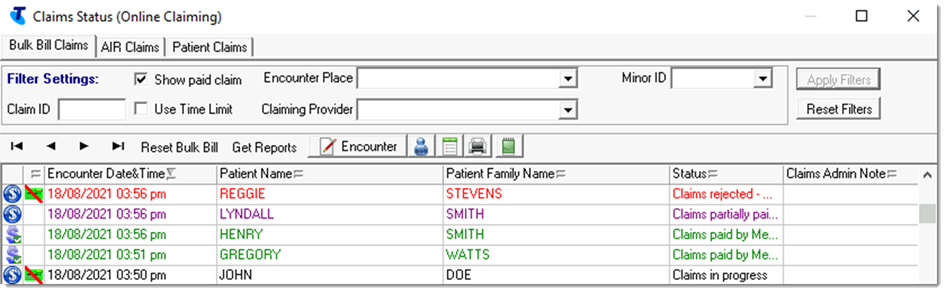
- Claim status icon and
Status - the current status
of the encounter claims. Multiple claim items for
one encounter may be included in one claim. Select
a claim to list the claim items separately.
Table 1. Online claiming - claims status Icon Status Description  |
| 
Claims in progress The claim has been sent or is in progress and there is not yet an outcome.
The claim may have failed validation: check the Result Text Message field and the Claim Status for more information.
For more information, see Troubleshooting online claims to Medicare.
If a claim remains in this status for more than 7 days, Reset Bulk Bill becomes available. Do not click Reset Bulk Bill except in consultation with Communicare Support or Medicare Australia.

Claims partially paid by Medicare Australia If all claim items are partially paid, the text is purple. If some claim items have different statuses, the text is black.
Review the Medicare report and the Service Record, where the status of individual items is displayed.
Tip: Click Encounter to open
the Service Record and amend the MBS items: for
example, deselect a failed item and select a more
appropriate item before claiming again. The whole
claim is resubmitted and Medicare identifies which
items are yet to be paid.
Encounter to open
the Service Record and amend the MBS items: for
example, deselect a failed item and select a more
appropriate item before claiming again. The whole
claim is resubmitted and Medicare identifies which
items are yet to be paid.For more information, see Troubleshooting online claims to Medicare.

Claim status unknown Claim is potentially claimable: the service has at least one provider with a provider number, but the claim has not been sent or marked as not claimable. For more information, see Troubleshooting online claims to Medicare.

Claims rejected - View Report Text is red.
Claim is not paid. As for partially paid claims, review the Medicare report and the Service Record and resubmit the claim if appropriate.
For more information, see Troubleshooting online claims to Medicare.

Claims paid by Medicare Australia Text is green.
Claim has been successfully paid. No further action is required.
- Information - for example,
 Medicare
Card details incomplete, displayed
for an encounter if the patient's Medicare Card
details are incomplete
Medicare
Card details incomplete, displayed
for an encounter if the patient's Medicare Card
details are incomplete - Encounter Date and Time - the start date and time of an encounter. If only the date is used, the date of the encounter.
- Patient Name - the patient's given names. If the patient is registered for HCH and the tier is recorded, the patient's HCH tier detail is highlighted.
- Patient Family Name - the patient's family name.
- Claims Admin Note -
click
 Admin Note to add or edit any notes associated
with the claim.
Admin Note to add or edit any notes associated
with the claim.
Filtering the encounters list
Set filters to limit the number of claims displayed.
- Apply one of more of the following filters:
- Claim ID - enter a
value to list claims that contain only the
specified claim ID. Enter as much of the claim ID
as required. For example,
P003 returns
P0031@,
P0031@...
P0039@.
To search for inpatient claim IDs, enter a search term starting with #. For example, #P003 returns #P0031@, #P0032@...#P0039@.
- Claiming Provider - select a provider from the list to display claims only for that specific provider
- Encounter Place - select an encounter place from the list to display claims only for a specific Encounter Place
- Show Paid Claim - set to display only paid claims. By default, Communicare displays only those claims that have not been paid.
- Use Time Limit - by default, only claims that are within the 2 year legal time limit imposed by Medicare Australia for electronically claimable services are displayed. Deselect to display all claims up to 50 years old.
- Minor ID - select a minor location ID from the list to display claims only for that location ID.
- Claim ID - enter a
value to list claims that contain only the
specified claim ID. Enter as much of the claim ID
as required. For example,
P003 returns
P0031@,
P0031@...
P0039@.
- Click Apply Filters.
Only those encounters that meet the filter criteria are displayed.
To display all encounters again, click Reset Filters.
Viewing and editing encounters
From the tab, you can edit encounters that haven't yet been sent or view them if they have. Typically, you would edit encounters that fail validation.
 Encounter - click
to open the service record where you can edit MBS
items associated with the service
Encounter - click
to open the service record where you can edit MBS
items associated with the service - click to edit patient details,
including specifying or updating a Medicare
number
- click to edit patient details,
including specifying or updating a Medicare
number - click to view the progress note
associated with the immunisation
- click to view the progress note
associated with the immunisation - click to print out a Medicare online
claiming bulk bill assignment of benefit form for
the selected patient
- click to print out a Medicare online
claiming bulk bill assignment of benefit form for
the selected patient  - click to add an administrative note
about the encounter
- click to add an administrative note
about the encounter
Bulk bill claims are automatically sent to Medicare by Communicare using Medicare Australia's online claiming when a service is complete.
Select an encounter from the encounters list to display information about the claims associated with that encounter in the claims list.
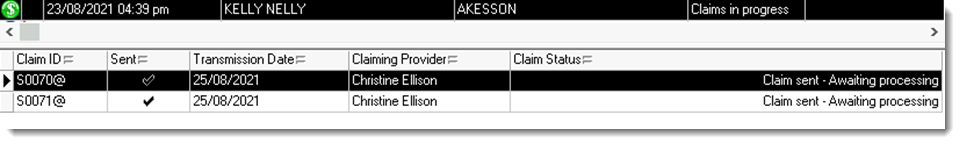
- Claim ID - unique identifier for a given month, which together with the date, identifies a claim within the online claiming system
- Sent - flag showing that the claim has been sent to Medicare Australia. If a claim is sent it cannot be modified.
- Transmission Date - the transmission date if the claim has been sent
- Claiming Provider - claiming provider for the claim
- Claim Status - current
state of the specific claim. A claim can have one
of the following states:
- Error: Claim not sent - please retry
- Claim waiting in queue
- Claim sent - Awaiting processing
- Claim processed - Awaiting Payment
- Claim paid by Medicare Australia
- Claim rejected - View Medicare Australia Report
- Claim discarded - when a rejected claim is retransmitted, the original claim is discarded
Claims are sent at the interval and times configured in CCareQueue_ServicesAustralia. By default, claims are sent hourly, 9:00-11:00am.
If a claim shows an error or is rejected, investigate the reason. If there is a problem with the patient or service record, correct it so that the claim can be resubmitted. For more information, see Working with submitted Medicare Claims.
Claim details
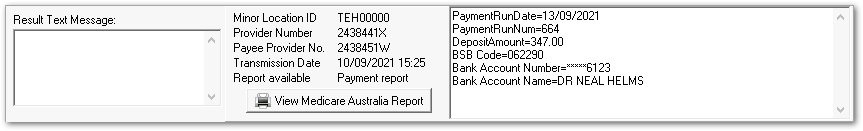
- Result Text Message - details of an attempt to process a claim returned by Services Australia or reasons for a failure to send. You can look up a Medicare reason code at PBS reason and rejection codes.
- Minor Location ID
- Provider Number
- Payee Provider No.
- Transmission Date - the date and time when this claim was transmitted to Medicare Australia if it was successfully transmitted
- Report available
- View Medicare Australia Report -
where there is a report
available, click to display information from
Medicare, including a Medicare -
Online Claiming Bulk Bill Report or
DB4 form received from Services Australia after a
claim is processed. Depending on whether the claim
has been fully processed and paid or not, the
available report will change. You may see either
of the following reports:
- Processing report - available where Medicare
has accepted the claim and started to process it.
Medicare may return a patient status code which
indicates problems with the Medicare card details
in the original claim. One of the following codes
may be displayed in the Medicare card
flag field:
- 8023 - patient identification amended
- 8024 - patient Medicare Issue number changed
- 8025 - patient Medicare Number changed
- 8026 - patient card will expire shortly
- 8027 - patient card expired. Future services may be rejected.
- 8028 - old Medicare Issue number for patient. Future services may be rejected.
- Payment report - available after Medicare has processed the claim and sent payment to the service provider. This report provides information about a service and its claim items. It includes details of payments deposited, a list of claims and transactions covered by the payment, explanations of all accepted and paid bulk bill claims, referral information, processing information and so on.
Note: If a claim does not progress from having a processing report to having a payment report, your local administrator should ensure that the Provider Number was correctly linked to the Minor ID at the time the claim was processed. Call Medicare eBusiness to check the status of the claim if you aren’t sure. - Processing report - available where Medicare
has accepted the claim and started to process it.
Medicare may return a patient status code which
indicates problems with the Medicare card details
in the original claim. One of the following codes
may be displayed in the Medicare card
flag field:
- Payment Details - details of payments made for a processed claim
Administrator jobs
Administrators should check Regular Administrator Tasks for details of online claiming maintenance.
